What Is A Soap Notes Template? Simplify Documentation
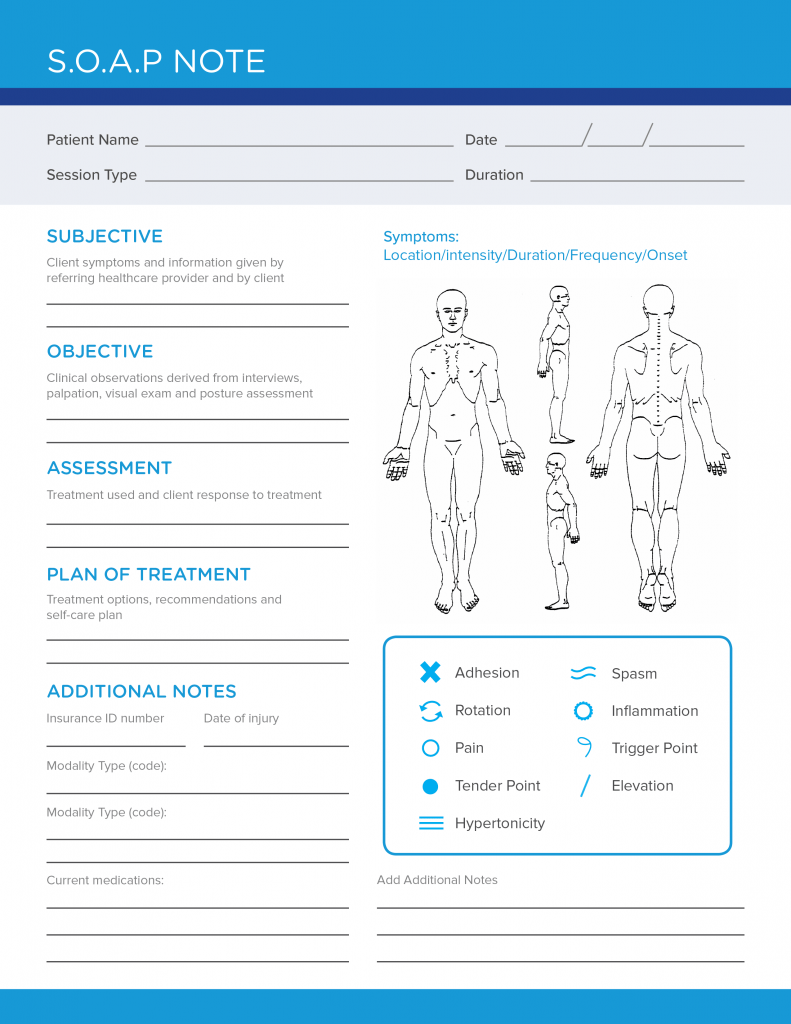
A SOAP notes template is a standardized method of documenting patient information in a clear and concise manner. SOAP is an acronym that stands for Subjective, Objective, Assessment, and Plan. This template is widely used in the medical field, particularly by healthcare professionals such as doctors, nurses, and therapists, to simplify documentation and ensure that all relevant information is captured during patient interactions.
Understanding the SOAP Notes Template
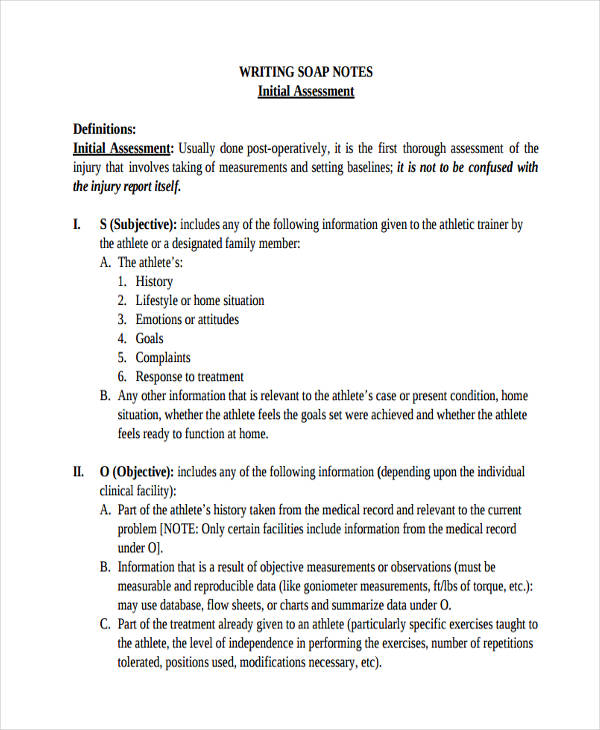
The SOAP notes template is divided into four main sections, each representing a different aspect of patient care. The sections are designed to be completed in a sequential manner, starting with the subjective information and ending with the plan for future care.
Subjective Section
The subjective section of the SOAP notes template is where healthcare professionals record the patient’s personal account of their symptoms, medical history, and concerns. This information is typically obtained through patient interviews and is essential for understanding the patient’s perspective and identifying potential health issues. The subjective section may include details such as:
- Chief complaint: The patient’s primary reason for seeking medical attention
- History of present illness: A detailed account of the patient’s symptoms and medical history
- Review of systems: A survey of the patient’s bodily systems to identify any potential health issues
Objective Section
The objective section of the SOAP notes template is where healthcare professionals record observable and measurable data about the patient’s condition. This information is typically obtained through physical examinations, laboratory tests, and other diagnostic procedures. The objective section may include details such as:
- Vital signs: The patient’s temperature, blood pressure, heart rate, and other vital signs
- Physical examination findings: The results of the physical examination, including any abnormal findings
- Laboratory and diagnostic test results: The results of any laboratory or diagnostic tests that have been performed
Assessment Section
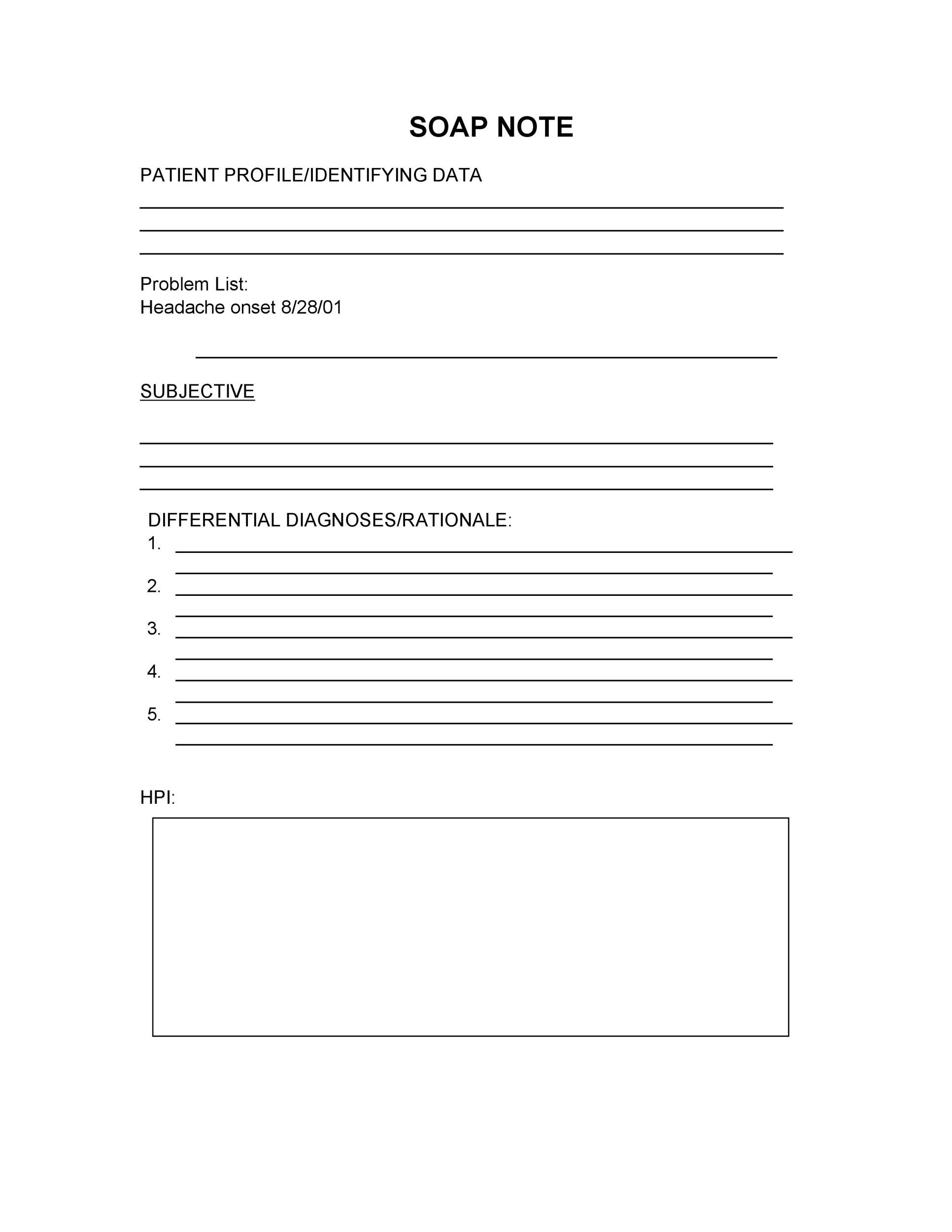
The assessment section of the SOAP notes template is where healthcare professionals summarize the patient’s condition and identify any potential health issues. This section is based on the information gathered in the subjective and objective sections and is used to develop a plan for future care. The assessment section may include details such as:
- Diagnosis: The healthcare professional’s diagnosis of the patient’s condition
- Differential diagnosis: A list of potential diagnoses that have been considered
- Identification of health issues: Any potential health issues that have been identified
Plan Section
The plan section of the SOAP notes template is where healthcare professionals outline the steps that will be taken to address the patient’s health issues. This section is based on the information gathered in the subjective, objective, and assessment sections and is used to develop a comprehensive plan for future care. The plan section may include details such as:
- Treatment options: The treatment options that will be used to address the patient’s health issues
- Medication: Any medications that will be prescribed to the patient
- Follow-up care: The plan for follow-up care, including any scheduled appointments or tests
| SOAP Section | Description |
|---|---|
| Subjective | Patient's personal account of symptoms and medical history |
| Objective | Observable and measurable data about the patient's condition |
| Assessment | Summary of the patient's condition and identification of potential health issues |
| Plan | Outline of the steps that will be taken to address the patient's health issues |
The use of a SOAP notes template can have a significant impact on patient care and outcomes. By providing a standardized method of documentation, SOAP notes templates can help healthcare professionals communicate more effectively and provide more comprehensive care. Additionally, SOAP notes templates can help healthcare professionals identify potential health issues earlier, which can lead to better patient outcomes and reduced healthcare costs.
Benefits of Using a SOAP Notes Template
There are several benefits to using a SOAP notes template, including:
- Improved communication: SOAP notes templates provide a standardized method of documentation, which can help healthcare professionals communicate more effectively
- Increased efficiency: SOAP notes templates can help healthcare professionals simplify documentation and reduce the time spent on paperwork
- Enhanced patient care: SOAP notes templates can help healthcare professionals provide more comprehensive care and identify potential health issues earlier
- Reduced errors: SOAP notes templates can help healthcare professionals reduce the risk of errors or omissions by providing a standardized method of documentation
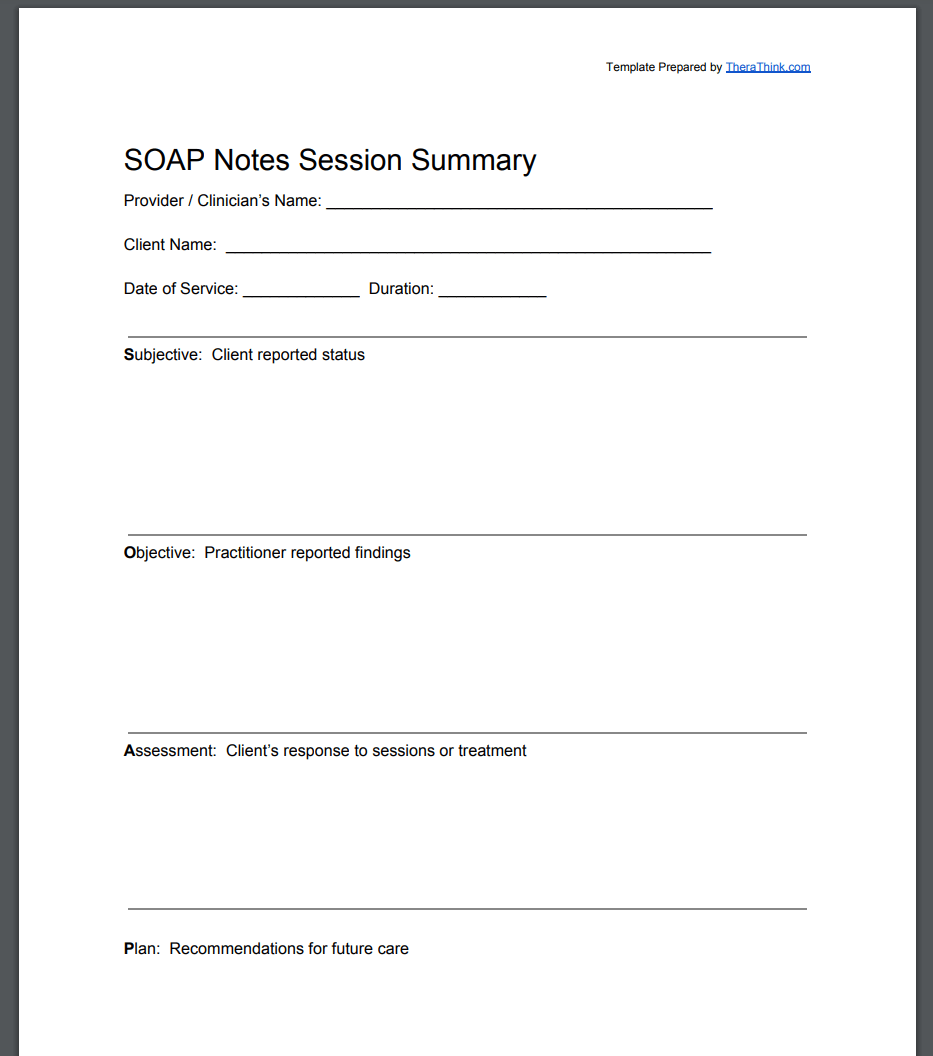
Examples of SOAP Notes Templates
There are many different types of SOAP notes templates that can be used in various healthcare settings. Some examples include:
- Medical SOAP notes template: This template is used in medical settings to document patient information and develop a plan for care
- Nursing SOAP notes template: This template is used in nursing settings to document patient information and develop a plan for care
- Therapy SOAP notes template: This template is used in therapy settings to document patient information and develop a plan for care
What is the purpose of a SOAP notes template?
+The purpose of a SOAP notes template is to provide a standardized method of documenting patient information and developing a plan for care. The template is designed to simplify documentation and ensure that all relevant information is captured during patient interactions.
How do I use a SOAP notes template?
+To use a SOAP notes template, simply fill out each section of the template with the relevant information. Start with the subjective section, followed by the objective section, assessment section, and plan section. Be sure to include all relevant information and follow the SOAP format to ensure that the template is completed correctly.
What are the benefits of using a SOAP notes template?
+The benefits of using a SOAP notes template include improved communication, increased efficiency, enhanced patient care, and reduced errors. The template provides a standardized method of documentation, which can help healthcare professionals communicate more effectively and provide more comprehensive care.
In conclusion, a SOAP notes template is a valuable tool for healthcare professionals that provides a standardized method of documenting patient information and developing a plan for care. By using a SOAP notes template, healthcare professionals can simplify documentation, improve communication, and provide more comprehensive care. Whether you are a doctor, nurse, or therapist, a SOAP notes template can help you provide high-quality patient care and reduce the risk of errors or omissions.