Did Trump Stop Medicaid
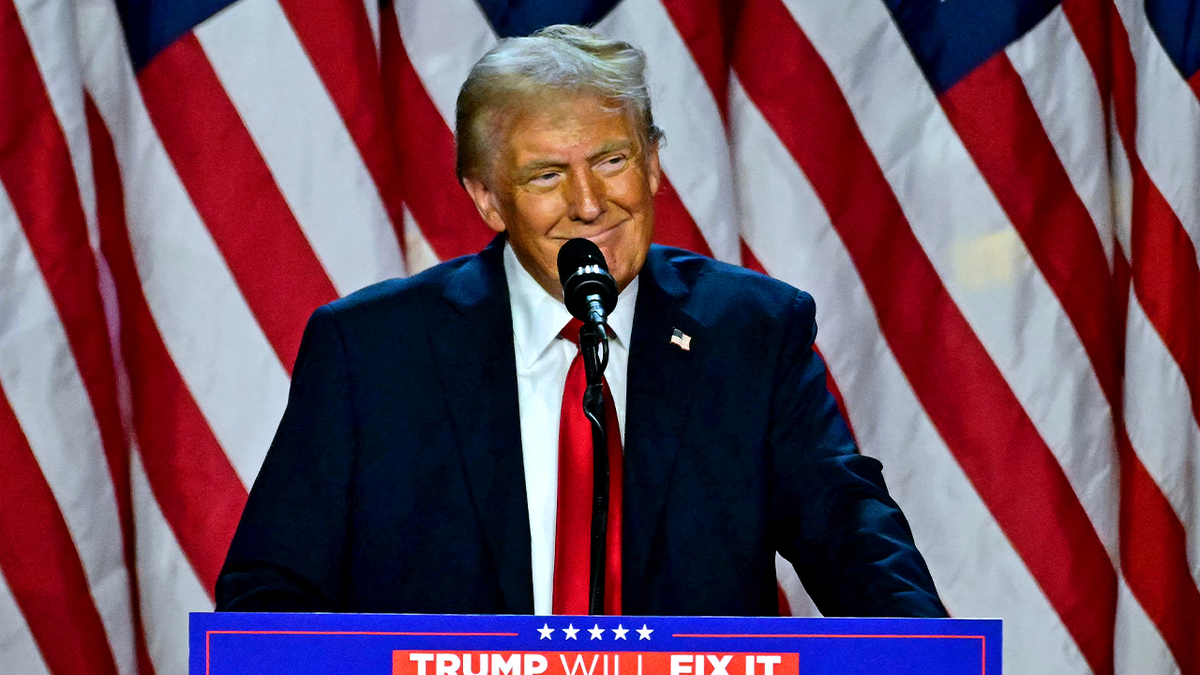
The question of whether former President Donald Trump stopped Medicaid is complex and requires an understanding of the actions his administration took regarding healthcare, particularly Medicaid, during his presidency. Medicaid is a federal and state program that provides health coverage to millions of Americans, including low-income adults, children, pregnant women, elderly adults, and people with disabilities.
Medicaid Expansion and the Trump Administration

The Trump administration did not completely stop Medicaid, but it did take several steps that affected the program’s reach and funding. One of the significant actions was the administration’s stance on the Medicaid expansion provision of the Affordable Care Act (ACA), also known as Obamacare. The ACA allowed states to expand Medicaid eligibility to include adults with incomes up to 138% of the federal poverty level, with the federal government covering a significant portion of the costs for the newly eligible population. Despite the ACA’s provision for Medicaid expansion, the Trump administration supported efforts to repeal and replace the ACA, which would have impacted Medicaid expansion.
Work Requirements and Medicaid
A notable policy change during the Trump administration was the approval of work requirements for Medicaid recipients in several states. The administration allowed states to impose work requirements on certain Medicaid beneficiaries as a condition of eligibility, arguing that this would encourage people to work and eventually move off Medicaid. Critics argued that such requirements would lead to eligible individuals losing coverage due to administrative barriers or because they were unable to meet the work requirements due to health issues or other challenges. By the end of Trump’s presidency, several states had implemented or were in the process of implementing these requirements, although court challenges and the COVID-19 pandemic paused or reversed some of these efforts.
| State | Work Requirement Implementation |
|---|---|
| Arkansas | Implemented in 2018, but later blocked by a federal court |
| Kentucky | Approved but never implemented due to legal challenges |
| Michigan | Implemented in 2020, but paused due to the COVID-19 pandemic |

Impact on Medicaid Enrollment and Access

The actions taken by the Trump administration, including support for repealing the ACA and implementing work requirements, had the potential to reduce Medicaid enrollment and access to healthcare for low-income individuals and families. However, the actual impact was mitigated by several factors, including court decisions blocking some of these policies and the COVID-19 pandemic, which led to an increase in Medicaid enrollment as more people became eligible due to job loss and decreased income.
COVID-19 Pandemic Response
During the COVID-19 pandemic, the Trump administration took steps to increase access to Medicaid, at least temporarily. The Families First Coronavirus Response Act (FFCRA) of 2020 included a provision that increased federal funding for Medicaid by 6.2 percentage points, but this increase was conditional on states not disenrolling current Medicaid beneficiaries unless they died, moved out of the state, or requested to be disenrolled. This policy helped maintain or increase Medicaid enrollment during the pandemic, ensuring that more people had access to healthcare services when they needed them most.
The response to the pandemic underscores the complex and sometimes contradictory nature of healthcare policy under the Trump administration, which at times sought to restrict Medicaid eligibility but also took actions to expand access during a public health crisis.
Did the Trump administration successfully repeal the Affordable Care Act?
+No, the Trump administration did not successfully repeal the Affordable Care Act. Despite several attempts, including legislative efforts and legal challenges, the ACA remains in place, although some of its provisions have been altered or challenged through administrative actions and court decisions.
How did work requirements affect Medicaid beneficiaries?
+The implementation of work requirements for Medicaid beneficiaries was intended to encourage work and reduce dependency on the program. However, critics and early data suggested that these requirements could lead to eligible individuals losing coverage, not necessarily because they found employment, but due to challenges in meeting the requirements or navigating the administrative process.
In summary, while the Trump administration did not stop Medicaid entirely, its policies and actions had significant implications for the program, including attempts to repeal the ACA, the introduction of work requirements, and responses to the COVID-19 pandemic. These efforts reflect the ongoing political and ideological debates about the role of Medicaid and the balance between providing healthcare coverage to vulnerable populations and promoting fiscal responsibility and personal responsibility.



